One-Size-Fits-None: Why It’s Time to Rethink Modern Medicine
One-Size-Fits-None: Why It’s Time to Rethink Modern Medicine

Let’s start with a bold thought: the future of medicine isn’t new—it’s ancient.
Once upon a time, medicine was deeply personal. The village healer, the traveling Chinese physician, or the old-school Western doctor didn’t treat “disease,” they treated you. They knew your lifestyle, your family, your environment. Medicine was tailored. The healer visited your home, examined your body, and prescribed a remedy made just for you.
Then came the industrial revolution—and with it, the rise of modern hospitals, pharmaceutical giants, and a system that traded personalized care for mass production. In the name of efficiency, medicine was standardized. Hospitals became the center of healing. Pills replaced potions. Pharmaceutical companies, empowered by economies of scale, began formulating “one-size-fits-all” treatments designed for populations, not individuals.
From a business standpoint, it was genius. From a patient’s perspective? Not always.

The Disruption Science Couldn’t Ignore
Thanks to the Human Genome Project and breakthroughs in pharmacogenomics, we now have clear scientific proof: people respond differently to drugs because of their unique genetic makeup. What works for one patient may be ineffective—or even harmful—for another.
One pill doesn’t fit all. And science proves it.
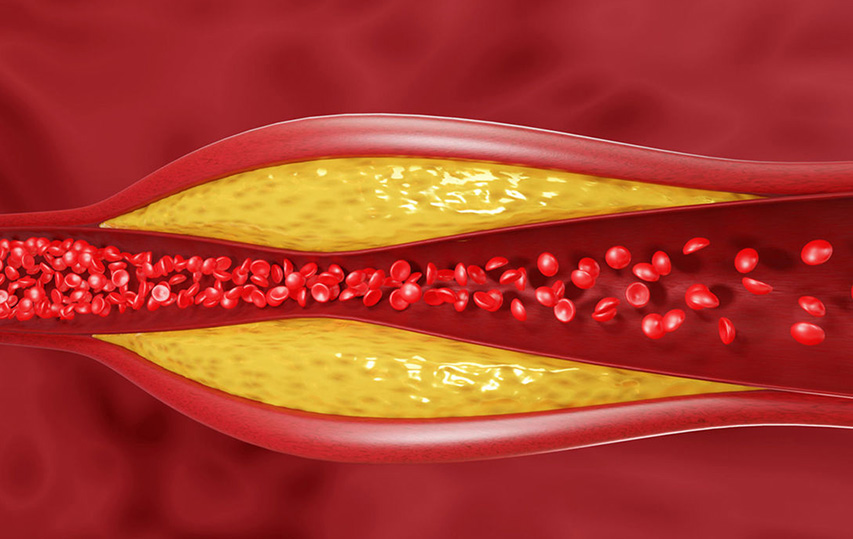
Yet the system resists change. Why? Because personalized medicine disrupts a business model that has worked—extremely profitably—for over a century. Pharmaceutical companies thrive on selling a single formulation to millions. Personalized treatment flips that model on its head. If every patient needs a unique formula based on their DNA, how can drug manufacturers keep costs low and profits high?
The Elephant in the Hospital Room
Today, doctors stand at the frontline of this conundrum. They’re often blamed when a drug causes side effects, doesn’t work, or—worst of all—harms the patient. In reality, the problem lies deeper: with a system built on generalization rather than individualization.
Take cancer care, for example. Many cancer drugs come with terrifying stories of side effects, complications, and even death—not because patients refused treatment, but because their bodies weren’t equipped to tolerate it. The trauma isn’t just physical—it’s emotional. The fear of becoming a victim of the treatment itself is very real.
Doctors wish for better tools—tools that align with modern science. They want to know, before prescribing, how a patient will respond. And that wish is becoming a reality.
Hope in Technology: Lessons from the Paint Store

Let me give you a real-world example.
Imagine walking into a paint store 30 years ago. You could only buy the popular colors of the season. Now? You can mix any shade you want, customized to your taste. The paint industry embraced on-demand technology, and it transformed customer satisfaction.
Why can’t we do the same with medicine?
With advances in 3D printing, AI, and pharmacogenomic profiling, we can. The idea of “N=1” (personalized treatment for a single patient) is no longer science fiction. It’s science waiting for the system to catch up.
We need a paradigm shift in how we think about healthcare—not just as a product to be sold, but as a service to be personalized.
Real Stories, Real Impact
Consider Emilia, a breast cancer patient who suffered debilitating side effects from chemotherapy. Standard dosing failed her. After a pharmacogenomic test revealed she had a gene variant that slowed drug metabolism, her oncologist adjusted her dose and treatment plan. The result? Improved outcomes, fewer side effects, and a patient who regained hope.
Or Mirzan, who had severe depression and spent years trying different antidepressants with no success. A simple genetic test showed that his liver lacked an enzyme needed to activate those drugs. Once he was switched to a medication suited to his profile, his symptoms finally improved.
These are not rare stories. They are the future of healthcare—if we let them be.

So, When Will This Happen?
It will happen when we, as patients, doctors, innovators, and policymakers, demand it.
It will happen when we stop asking, “What’s the most common treatment?” and start asking, “What’s the right treatment for me?”
It will happen when we realize that efficiency should never trump efficacy, and that the purpose of medicine isn’t to treat diseases—it’s to heal people.
We must challenge the conventional. We must think beyond the pill. We must return to wisdom—but this time, backed by science.
Personalized medicine isn’t the future. It’s a return to the past—with better tools.
And it’s time we brought humanity back into healthcare.